Reverse Shoulder Arthroplasty
The Goal
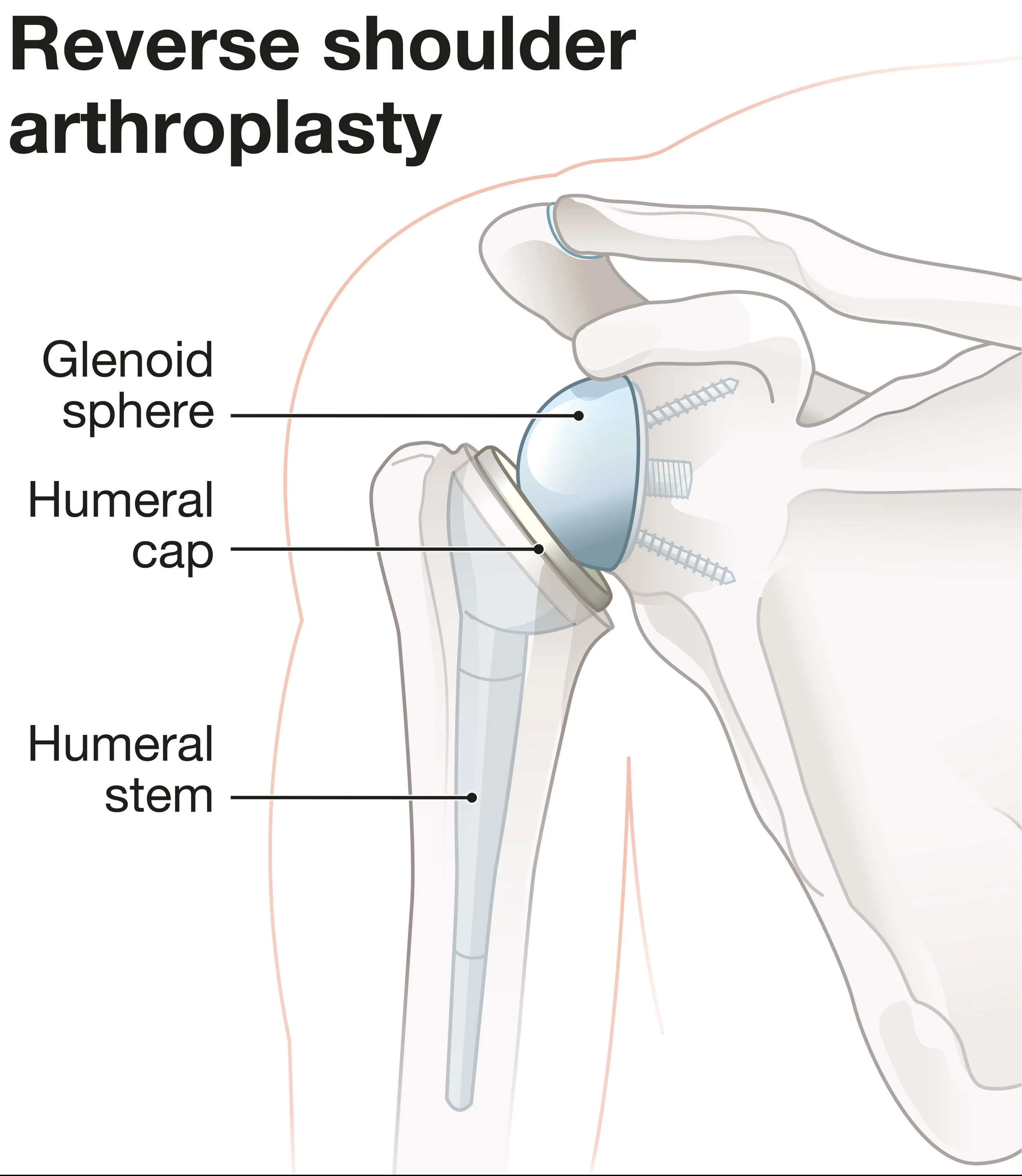
Dr. Kevin Wall provides specialized, fellowship-trained surgical treatment for Reverse Shoulder Arthroplasty (RSA) to restore function and relieve pain for patients in Richmond, VA, and the surrounding Central Virginia communities. The original goal of this procedure is to restore the ability to lift the arm in patients who have developed "cuff tear arthropathy"—a specific type of shoulder arthritis caused by a massive, irreparable rotator cuff tear. In a normal ball and socket shoulder, the rotator cuff powers arm elevation. When it is torn, the arm cannot be lifted (pseudoparalysis) and the joint wears out. The "reverse" replacement switches the anatomy: the ball is replaced with a socket and the socket is replaced with a ball. This unique mechanical design bypasses the non-functioning rotator cuff and recruits the deltoid muscle to become the new engine of the shoulder, restoring overhead function and eliminating pain.
Recently the reverse replacement has been used for progressively more conditions, though the mechanics and rationale of providing a strong, durable shoulder remain the same. Reverse shoulder arthroplasty is also often recommended for: rotator cuff tears in the elderly even without formal cuff tear arthropathy changes, proximal humerus fractures, and as the revision option when anatomic total shoulder arthroplasties or hemiarthroplasties fail.
This page is designed to educate you specifically about this procedure. Additional information that generally applies to most of Dr. Wall’s surgeries can be found on these pages:
For more information on this topic, see the American Academy of Orthopaedic Surgeon's educational page here.
For more information on living with a joint replacement, see the American Academy of Orthopaedic Surgeon's educational page here.
For an example video of this procedure, see the American Academy of Orthopaedic Surgeon's educational page here.
The Procedure
The Approach: Performed through a standard deltopectoral incision on the front of the shoulder to expose the joint while protecting the deltoid muscle.
Component Reversal: Unlike a standard replacement, Dr. Wall implants a polished metal sphere (glenosphere) onto your natural socket and a high-density polyethylene cup onto the top of your humerus.
Restoring Tension: The implant is carefully tensioned to lengthen the deltoid muscle, giving it the mechanical advantage needed to lift the arm without the help of the rotator cuff.
Biologic Fixation: The components are typically "press-fit" into the bone, allowing your own bone to grow into the metal for a permanent, biologic bond.
Post-Op Protocol
Start Formal PT: Professional physical therapy sessions begins immediately.
Phase 1 (0–4 weeks): Sling: You must wear the sling at all times unless performing hygiene or prescribed exercises. Gentle passive range of motion (PROM) including pendulums is allowed. No active motion of the shoulder is permitted. You may move your elbow, wrist, and hand as tolerated. No lifting, pushing, pulling, or weightbearing.
Phase 2 (4–6 weeks): Weaning: You will begin weaning from the sling. Progression to passive, active-assisted, and active motion as tolerated. Periscapular strengthening begins. You may lift light objects weighing 1–2 pounds (e.g., a cup of coffee). No pushing or pulling.
Phase 3 (6–8 weeks): Progression: Continue advancing range of motion. Gradual internal rotation (IR) is introduced. Continue periscapular and deltoid strengthening.
Phase 4 (8–12 weeks): Achieve full range of motion. You may now lift up to 10 pounds.
Phase 5 (12–16 weeks): Continued strengthening. You may now lift up to 15 pounds.
Phase 6 (16+ weeks): * Return to Activity: Return to labor-intensive work or recreational sports. You may progress to higher weights as tolerated, de-escalating if heavier loads cause pain.
When to Seek Care
You should schedule a consultation if:
You have been told you have a "massive" rotator cuff tear and arthritis.
You had a recent fall and shoulder dislocation.
You have been told you have a proximal hummerus fracture.
You are unable to lift your arm above shoulder height (pseudoparalysis), even though you still have feeling in the arm.
You have had a previous rotator cuff repair that failed and is now painful.
You have had a previous shoulder replacement that is now painful and you are losing motion.