Anatomic Total Shoulder Arthroplasty
The Goal
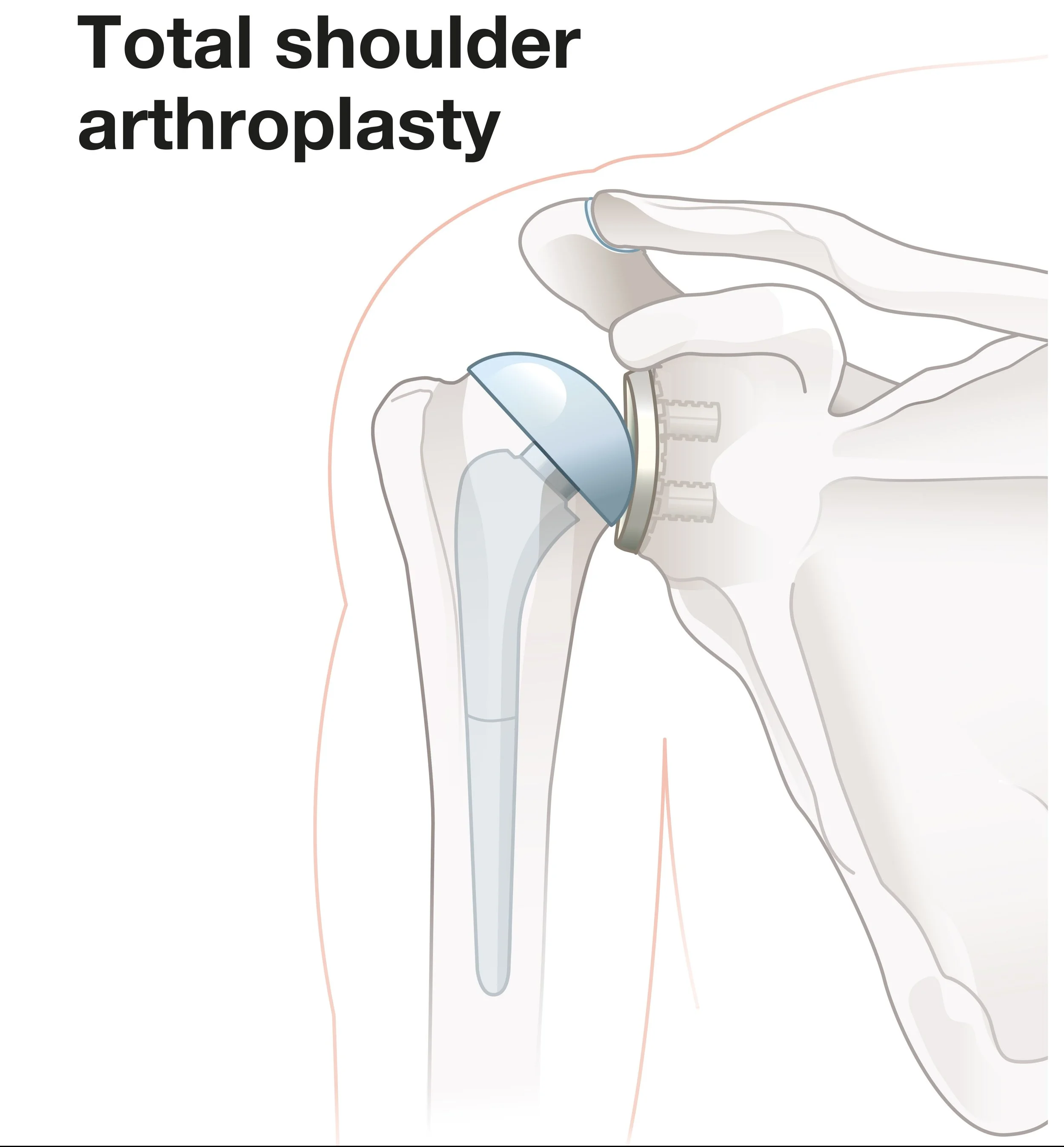
Dr. Kevin Wall provides specialized, fellowship-trained surgical treatment for Anatomic Total Shoulder Arthroplasty to restore function and relieve pain for patients in Richmond, VA, and the surrounding Central Virginia communities. To eliminate the debilitating pain of "bone-on-bone" shoulder arthritis while preserving the natural mechanics of the joint. The goal of an anatomic replacement is to restore a smooth gliding surface using a highly polished metal ball and a durable plastic socket. Unlike a reverse replacement, this procedure relies on your native rotator cuff to move the arm. In an anatomic total shoulder arthroplasty the ball (humeral head) is replaced with a ball, and the socket (glenoid) is replaced with a socket). By accurately recreating your unique anatomy, we aim to restore a nearly full range of motion and independent function for activities of daily living.
This page is designed to educate you specifically about this procedure. Additional information that generally applies to most of Dr. Wall’s surgeries can be found on these pages:
For more information this procedure, see the American Academy of Orthopaedic Surgeon's educational page here.
For more information on living with a joint replacement, see the American Academy of Orthopaedic Surgeon's educational page here.
For an example video of this procedure, see the American Academy of Orthopaedic Surgeon's educational page here.
The Procedure
3D Guided Planning: Prior to surgery, Dr. Wall utilizes 3D CT reconstructions to map your specific bone structure, allowing for precise positioning of the implants.
The Approach: Performed through a deltopectoral incision on the front of the shoulder, utilizing the natural interval between muscles to minimize tissue trauma. The subscapluaris tendon (one of the rotator cuff muscles) is carefully removed from the front of the humerus to gain access to the shoulder joint.
Resurfacing: The arthritic humeral head is removed and replaced with a metal prosthesis, while the glenoid is fitted with a cemented polyethylene (plastic) liner.
Anatomic Repair: The subscapularis is securely reattached to its original footprint with high-strength sutures, which is critical for restoring stability and internal rotation strength.
Post-Op Protocol
Immobilization: Use a sling as needed during the day and wear it consistently at night for the first 4 weeks. The sling may be removed for hygiene and to perform elbow, wrist, and hand exercises as tolerated. Weaning from the sling typically begins between weeks 4 and 6.
Early Motion: Formal physical therapy begins at post-operative week 0. Initial therapy focuses on passive and active-assisted range of motion (PROM/AAROM) and scapular strengthening. External rotation is strictly limited to 30 degrees during Phase 1 to protect the subscapularis repair.
Restrictions: No active range of motion, pushing, pulling, or weightbearing for the first 4 weeks. From weeks 4 to 6, pushing, pulling, and weightbearing are limited to no more than 1–2 pounds (roughly the weight of a cup of coffee). Lifting capacity increases to 10 pounds between weeks 6 and 12.
Recovery: Progressive active motion and strengthening continue through week 12. A discussion regarding return to labor or recreational sports typically occurs at the 16-week mark.
When to Seek Care
You should schedule a consultation if:
You hear or feel a 'grinding' or 'catching' sensation in the joint.
You have lost significant range of motion (e.g., cannot reach behind your back or overhead).
Conservative treatments like cortisone shots or physical therapy are no longer providing relief.