Pectoralis Major Repair
The Goal
Dr. Kevin Wall provides specialized, fellowship-trained surgical treatment for Pectoralis Major Repair to restore function and relieve pain for patients in Richmond, VA, and the surrounding Central Virginia communities. The goal of this procedure is to restore the strength and cosmetic appearance of the chest following a rupture of the pectoralis major tendon. This injury is most common in weightlifters (often occurring during a bench press) and contact athletes. A complete tear results in a loss of adduction and internal rotation strength, as well as a visible deformity where the muscle belly retracts toward the center of the chest. Surgical repair reattaches the torn tendon to its native footprint on the humerus, restoring the "axillary web" and allowing patients to return to high-demand activities.
This page is designed to educate you specifically about this procedure. Additional information that generally applies to most of Dr. Wall’s surgeries can be found on these pages:
The Procedure
The Approach: Performed through an open incision in the deltopectoral interval or slightly more axillary (armpit) based to access the retracted tendon.
Tendon Mobilization: The torn tendon is identified, which often involves dissecting it free from scar tissue if the injury is chronic.
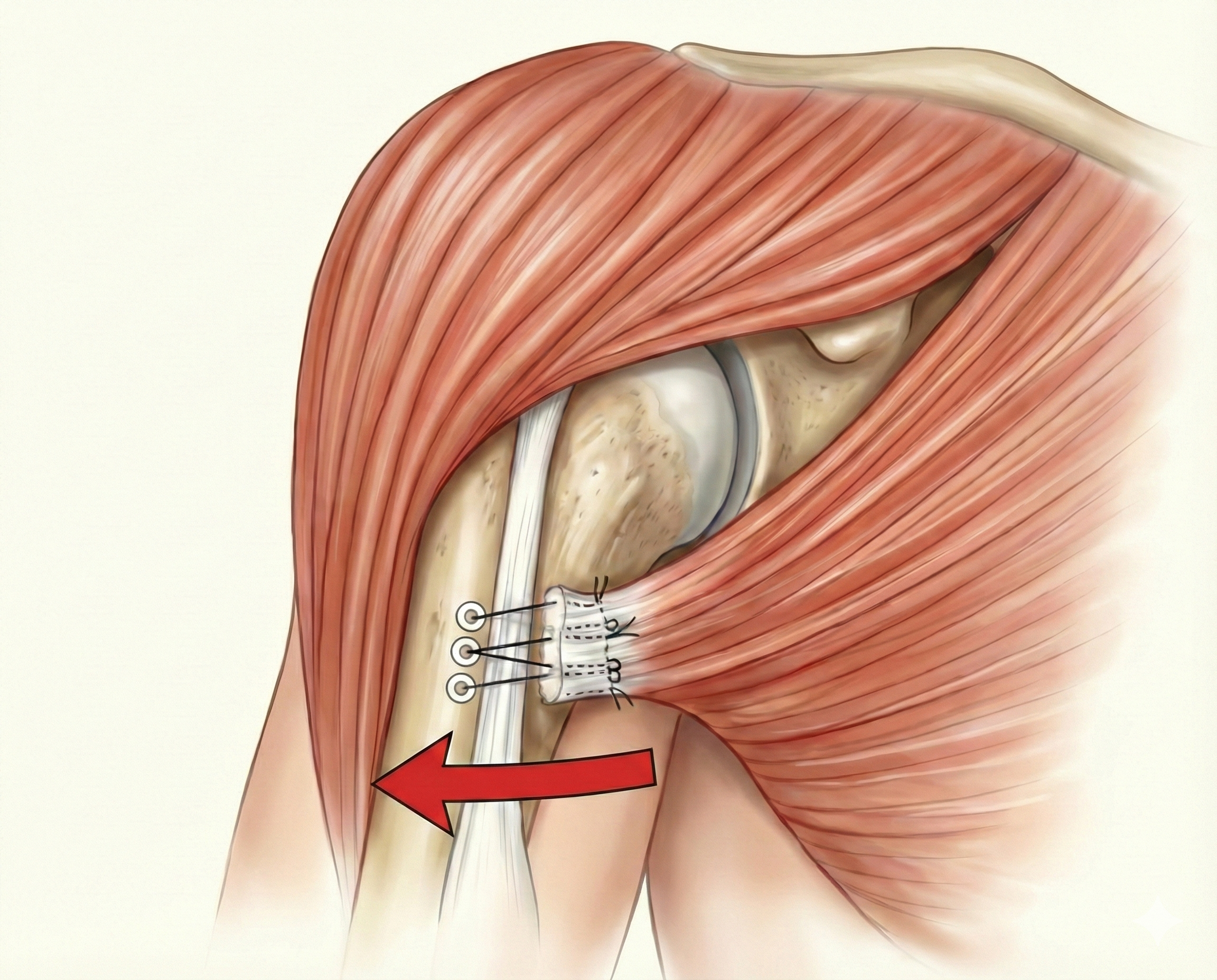
Fixation:
Acute Repairs: High-strength sutures are woven through the tendon end. These are then secured to the humerus bone using cortical buttons or heavy-duty suture anchors.
Chronic/Retracted Tears: If the tendon cannot reach the bone due to retraction, an allograft (donor tissue) may be used to bridge the gap and reconstruct the connection.
Post-Op Protocol
Immobilization (Phase 1: 0–4 weeks): You must remain in a sling at all times, except for hygiene and physical therapy. Formal physical therapy begins at Week 2.
Exercises: Gentle, progressive passive range of motion (PROM) of the shoulder and scapular strengthening (Week 3).
Restrictions: No pushing, pulling, or weightbearing.
Phase 2 (4–6 weeks): You will begin weaning from the sling (completed by Week 4 for bone-tendon repairs; Week 6 for tendon-tendon/allograft repairs).
Exercises: Continue scapular strengthening. Progress to active-assisted range of motion (AAROM).
Phase 3 (6–8 weeks): Gradual weightbearing may begin. You will progress to full active range of motion (AROM).
Phase 4 (8–14 weeks): The goal is to achieve full range of motion by Week 14. Strengthening exercises are progressively advanced.
Phase 5 (14–20+ weeks): Continued strengthening. Return to heavy lifting or sport is determined based on strength testing and tissue quality.
When to Seek Care
You should schedule a consultation if:
You felt a sharp "rip" or tearing sensation in your chest or armpit while bench pressing.
You have significant bruising on your upper arm and chest wall.
You notice that your chest muscle or armpit looks uneven.