Arthroscopic Capsular Release
The Goal
Dr. Kevin Wall provides specialized, fellowship-trained surgical treatment for Arthroscopic Capsular Release to restore function and relieve pain for patients in Richmond, VA, and the surrounding Central Virginia communities.
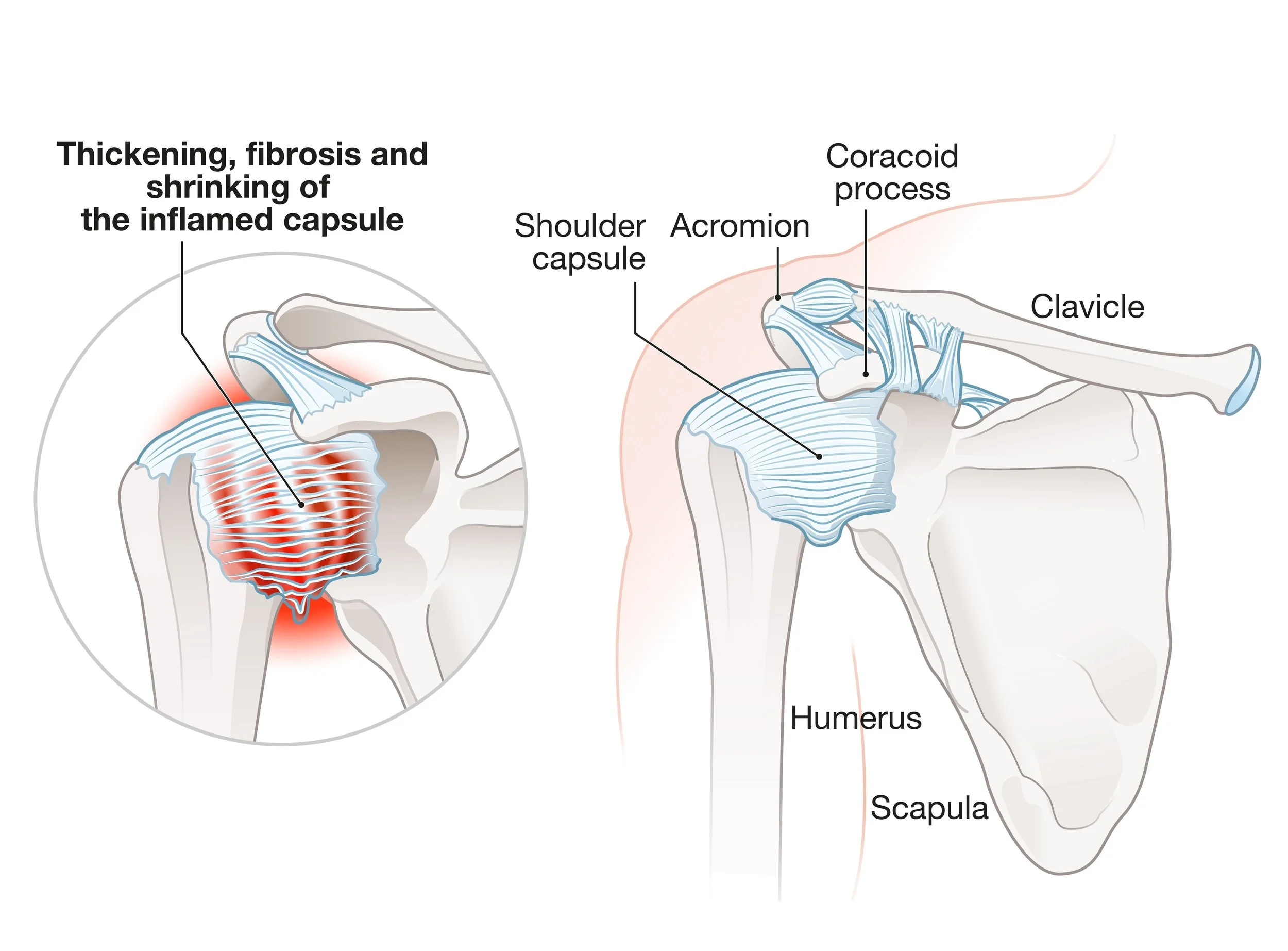
The goal of this procedure is restore range of motion and eliminate the debilitating pain associated with "frozen shoulder" (adhesive capsulitis). In this condition, the joint capsule becomes severely inflamed, scarred, and contracted, which physically prevents the shoulder from moving. When non-surgical solutions like targeted injections and specific stretching fail to "cool down" the joint, a surgical release is performed to mechanically divide these tight tissues and restore the shoulder's natural mobility. This procedure is also frequently performed in conjuction with other arthroscopic procedures such as rotator cuff repairs.
This page is designed to educate you specifically about this procedure. Additional information that generally applies to most of Dr. Wall’s surgeries can be found on these pages:
The Procedure
The Approach: Performed arthroscopically (minimally invasive) under general anesthesia using 2–3 small incisions.
Surgical Division: Dr. Wall precisely divides the contracted anterior capsule within the "rotator interval," the primary area of thickening in frozen shoulder cases. When indicated the rest of the capsule (superior, posterior and inferior) can also be carefully divided. Great care is taken to protect the axillary nerve, just under the inferior capsule
Manipulation: After the mechanical release, the shoulder is gently manipulated to stretch any remaining bands of scarred tissue.
Integrated Pain Control: To ensure patients can begin moving comfortably right away, an interscalene catheter nerve block by the anesthesia team is preferred for continuous local anesthetic for the first few days after surgery.
Post-Op Protocol
Immobilization: A sling is used for comfort during the first few days only. Immobilization any longer than this must be avoided to prevent the joint from re-stiffening.
Early Motion (Days 1–10): Formal physical therapy begins within 1–2 days of surgery. In this "Immediate Post-Op Phase," you should see your therapist 3–5 times per week. The focus is on passive stretching to keep the motion restored during surgery.
Home Exercise Program: Success depends on high-frequency stretching. You will perform pendulums, supine external rotation, and passive arm elevation 4–5 times per day.
Phase 2 (Weeks 3–6): Transition to active-assisted motion. You can begin using the arm for light daily activities (eating, typing, dressing) as tolerated. Swimming is encouraged at this phase and beyond.
Phase 3 (Weeks 6+): Once full, painless range of motion has been regained, proressive strengthening and return to recreational activities may occur.
When to Seek Care
You should schedule a consultation if:
You have a progressive loss of motion in all directions, not just one.
You experience "thawing" pain—sharp, intense pain occurring with any sudden movement.
You find it increasingly difficult to reach into your back pocket or put on a coat.